
School is back in session, and a first-of-its-kind class has begun in Grande Prairie, training future physicians in the north.
The Northern Alberta Medical Program (NAMP) celebrated the first day of classes on Tuesday with its first cohort of 30 students.
“I don't know if you realize how historic this is actually going to be; this is going to transform medicine in northern Alberta,” said Adriana LaGrange, Minister of Primary and Preventive Health Services, at a ceremony before students began classes.

She said it’s the beginning of a new era of medical education and healthcare in northern Alberta.
Students will complete their first two years of the MD program at Northwestern Polytechnic’s (NWP) Health Education Centre (HEC) in the Grande Prairie Regional Hospital (GPRH).
After the first two years, students will have clerkship placements across northern Alberta and in northern communities in the Yukon and Northwest Territories.
Students will earn their MD through the University of Alberta and participate in the same training as medical students in Edmonton.
“It is an innovative approach to medical education that will help address rural physician shortages, and is one of many ways we are implementing solutions to physician shortages,” said LaGrange.
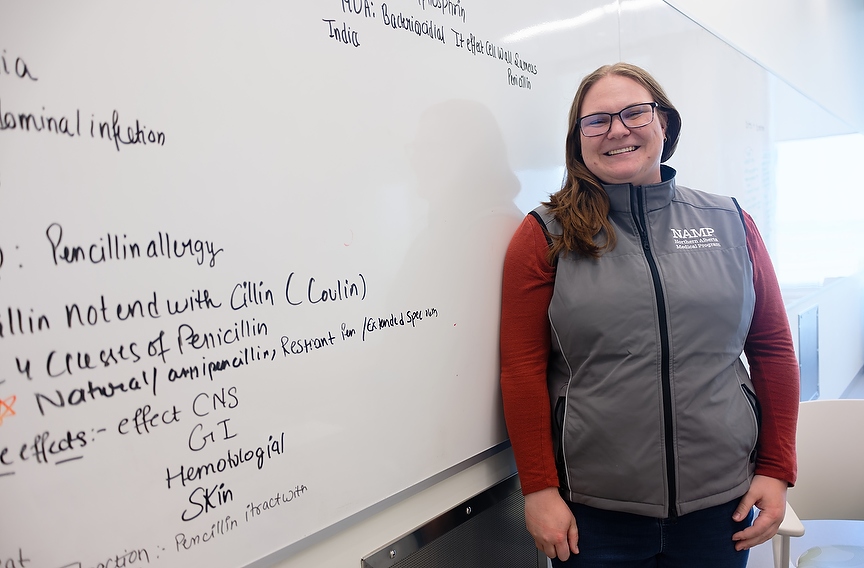
Grande Prairie resident Megan Hopkins is part of the first cohort of NAMP students.
“I was working here at the GPRH in the emergency room, I really saw the gap that we currently have in health care, where so many of those visits could have been prevented if people had a primary care physician,” she said.
Hopkins, a pharmacist, seized the opportunity to study in her hometown, aiming to be “more hands-on” in helping her community.
“Rural is where I'm most comfortable; as a pharmacist, I practiced in both the city and rurally, so being able to practice in that setting is definitely a big deal for me.”
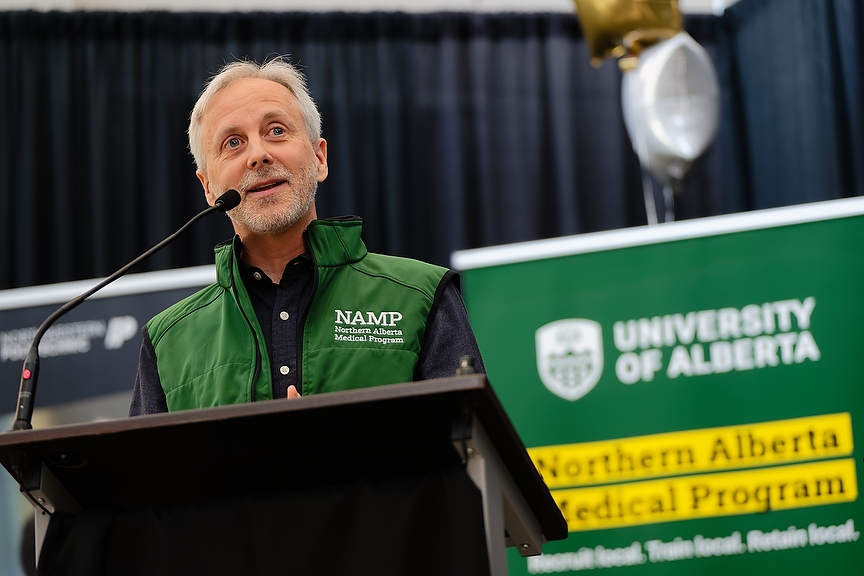
Twenty of the 30 students come from a rural background with the remainder from an urban centre such as Calgary or Edmonton, said NAMP Assistant Dean Richard Martin.
“One thing I've learned along the way is that you don't need to actually come from a rural space to feel like this is the work that's meaningful for you.”
Martin said he grew up in Edmonton and completed his medical schooling there. While doing his residency it was suggested he try two weeks in Whitecourt.
“It showed me very quickly that the style of work they were doing was absolutely the style of work that I wanted to do, and actually, from the time I left that experience in Whitecourt, there was no other choice in my mind for what I was going to do.”
He ended up working in Whitecourt after his schooling and then eventually moved to Grande Prairie to begin practicing.
“What the students are learning, as far as details, is really the same (as Edmonton) because being a doctor in Edmonton is really the same kind of work as being a doctor in Grande Prairie,” Martin said.
An advantage of training physicians locally is that they will gain a deeper understanding of what it means to work in a rural setting, interacting with patients, families and the community.
He said that during the first two years of training, students will learn in a small group and lecture format, with some contact with patients and clinical work.
While in the third and fourth year, students will be learning “directly by helping take care of patients and families, working with physicians and nurses and paramedicine across the landscape of where they are.”
He said in those final two years, the students will be found anywhere a physician can be found, including hospitals, clinics, ambulances and long-term care facilities.
The hope is that by recruiting and training locally, NAMP will retain physicians in the region.
“We definitely want that to happen, and it is because students who learn in rural communities are more likely to stay and work in rural areas after completing their training,” said LaGrange.
She said the same concept has been successful in the education sector.
“We saw this in education. I was the education minister for K to 12 education for four years, and we saw that roughly about 70 per cent of teachers trained in rural communities actually stayed there.”
She said the province recognizes “there are physician shortages in rural and remote communities” and it's taking action with programs like NAMP.

In April last year, the province invested over $224 million into physician training at NWP and the University of Lethbridge. In the same month, U of A and NWP signed a Memorandum of Understanding, formally uniting the institutions to bring physician training to Grande Prairie.
“The arrival of the first cohort of medical students in Grande Prairie is historic, not only for medical education in Alberta, but it also serves as a powerful symbol of hope for the communities in northern Alberta,” said NWP president Vanessa Sheane.
“We know that health care and post-secondary education in the north are complex and continually evolving, but today we stand together as proof of what can be achieved with vision, collaboration and determination aligned.”

Minister of Advanced Education Myles McDougall said the program’s success is due to the collaboration between the U of A and NWP.
“Grande Prairie has this reputation to get things done,” he said.
Although the halls of the HEC were full of past and current politicians, advocates, and community leaders, Hopkins - on her first day of classes - was excited to show her classmates all that the north has to offer.